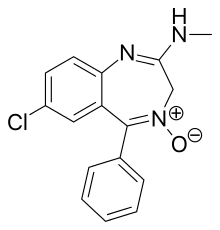
Chlordiazepoxide
Chlordiazepoxide
Jump to navigation
Jump to search
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌklɔːrdaɪ.əzɪˈpɒksaɪd/ |
| Trade names | Librium |
AHFS/Drugs.com | Monograph |
| MedlinePlus | a682078 |
| Pregnancy category |
|
| Routes of administration | oral intramuscular |
| ATC code |
|
| Legal status | |
| Legal status |
|
Pharmacokinetic data | |
| Metabolism | Hepatic |
| Elimination half-life | 5–30 hours (Active metabolite desmethyldiazepam 36–200 hours: other active metabolites include oxazepam) |
| Excretion | Renal |
| Identifiers | |
IUPAC name
| |
| CAS Number |
|
PubChem CID |
|
| IUPHAR/BPS |
|
| DrugBank |
|
| ChemSpider |
|
| UNII |
|
| KEGG |
|
| ChEBI |
|
| ChEMBL |
|
| ECHA InfoCard | 100.000.337 |
| Chemical and physical data | |
| Formula | C16H14ClN3O |
| Molar mass | 299.75 g/mol |
| 3D model (JSmol) |
|
SMILES
| |
InChI
| |
.mw-parser-output .nobold{font-weight:normal} (verify) | |
Chlordiazepoxide, trade name Librium, is a sedative and hypnotic medication of the benzodiazepine class; it is used to treat anxiety, insomnia and withdrawal symptoms from alcohol and/or drug abuse.
Chlordiazepoxide has a medium to long half-life but its active metabolite has a very long half-life. The drug has amnesic, anticonvulsant, anxiolytic, hypnotic, sedative and skeletal muscle relaxant properties.[1]
Chlordiazepoxide was discovered in 1959.[2] It was the first benzodiazepine to be synthesized and the discovery of chlordiazepoxide was by pure chance.[3] Chlordiazepoxide and other benzodiazepines were initially accepted with widespread public approval but were followed with widespread public disapproval and recommendations for more restrictive medical guidelines for its use.[4]
Contents
1 Medical uses
2 Contraindications
2.1 Pregnancy
3 Adverse effects
3.1 Tolerance and dependence
3.1.1 Tolerance
3.1.2 Dependence
3.2 Overdose
4 Interactions
5 Pharmacology
6 Pharmacokinetics
7 History
8 Recreational use
8.1 Legal status
9 Toxicity
9.1 Animal
10 Availability
11 See also
12 References
13 External links
Medical uses[edit]
Chlordiazepoxide is indicated for the short-term (2–4 weeks) treatment of anxiety that is severe and disabling or subjecting the person to unacceptable distress. It is also indicated as a treatment for the management of acute alcohol withdrawal syndrome.[5]
It can sometimes be prescribed to ease symptoms of irritable bowel syndrome combined with clidinium bromide as a fixed dose medication, Librax.[6]
Contraindications[edit]
Use of chlordiazepoxide should be avoided in individuals with the following conditions:
- Myasthenia gravis
- Acute intoxication with alcohol, narcotics, or other psychoactive substances
- Ataxia
- Severe hypoventilation
- Acute narrow-angle glaucoma
- Severe liver deficiencies (hepatitis and liver cirrhosis decrease elimination by a factor of 2)
- Severe sleep apnea
- Hypersensitivity or allergy to any drug in the benzodiazepine class
Chlordiazepoxide is generally considered an inappropriate benzodiazepine for the elderly due to its long elimination half-life and the risks of accumulation.[7] Benzodiazepines require special precaution if used in the elderly, pregnancy, children, alcohol- or drug-dependent individuals and individuals with comorbid psychiatric disorders.[8]
Pregnancy[edit]
The research into the safety of benzodiazepines during pregnancy is limited and it is recommended that use of benzodiazepines during pregnancy should be based on whether the benefits outweigh the risks. If chlordiazepoxide is used during pregnancy the risks can be reduced via using the lowest effective dose and for the shortest time possible. Benzodiazepines should generally be avoided during the first trimester of pregnancy. Chlordiazepoxide and diazepam are considered to be among the safer benzodiazepines to use during pregnancy in comparison to other benzodiazepines. Possible adverse effects from benzodiazepine use during pregnancy include, abortion, malformation, intrauterine growth retardation, functional deficits, carcinogenesis and mutagenesis. Caution is also advised during breast feeding as chlordiazepoxide passes into breast milk.[9][10]
Adverse effects[edit]
Sedative drugs and sleeping pills, including chlordiazepoxide, have been associated with an increased risk of death.[11]
Common side-effects of chlordiazepoxide include:[12]
- Confusion
- Constipation
- Drowsiness
- Fainting
- Altered sex drive
- Liver problems
- Lack of muscle coordination
- Minor menstrual irregularities
- Nausea
- Skin rash or eruptions
- Swelling due to fluid retention
- Yellow eyes and skin
Chlordiazepoxide in laboratory mice studies impairs latent learning. Benzodiazepines impair learning and memory via their action on benzodiazepine receptors, which causes a dysfunction in the cholinergic neuronal system in mice.[13] It was later found that scopolamine impairment in learning was caused by an increase in benzodiazapine/GABA activity (and that benzodiazepines were not associated with the cholinergic system).[14] In tests of various benzodiazepine compounds, chlordiazepoxide was found to cause the most profound reduction in the turnover of 5HT (serotonin) in rats. Serotonin is closely involved in regulating mood and may be one of the causes of feelings of depression in rats using chlordiazepoxide or other benzodiazepines.[15]

Tolerance and dependence[edit]
Tolerance[edit]
Chronic use of benzodiazepines, such as chlordiazepoxide, leads to the development of tolerance, with a decrease in number of benzodiazepine binding sites in mouse forebrain.[16] The Committee of Review of Medicines, who carried out an extensive review of benzodiazepines including chlordiazepoxide, found - and were in agreement with the Institute of Medicine (USA) and the conclusions of a study carried out by the White House Office of Drug Policy and the National Institute on Drug Abuse (USA) - that there was little evidence that long-term use of benzodiazepines were beneficial in the treatment of insomnia due to the development of tolerance. Benzodiazepines tended to lose their sleep-promoting properties within 3–14 days of continuous use, and in the treatment of anxiety the committee found that there was little convincing evidence that benzodiazepines retained efficacy in the treatment of anxiety after 4 months' continuous use due to the development of tolerance.[17]
Dependence[edit]
Chlordiazepoxide can cause physical dependence and what is known as the benzodiazepine withdrawal syndrome. Withdrawal from chlordiazepoxide or other benzodiazepines often leads to withdrawal symptoms that are similar to those seen with alcohol and barbiturates. The higher the dose and the longer the drug is taken, the greater the risk of experiencing unpleasant withdrawal symptoms. Withdrawal symptoms can, however, occur at standard dosages and also after short-term use. Benzodiazepine treatment should be discontinued as soon as possible through a slow and gradual dose-reduction regime.[18]
Chlordiazepoxide taken during pregnancy can cause a postnatal benzodiazepine withdrawal syndrome.[19]
Overdose[edit]
An individual who has consumed excess chlordiazepoxide may display some of the following symptoms:
Somnolence (difficulty staying awake)- Mental confusion
- Hypotension
- Hypoventilation
- Impaired motor functions
- Impaired reflexes
- Impaired coordination
- Impaired balance
- Dizziness
- Muscle weakness
- Coma
In animal models, the oral median lethal dose of chlordiazepoxide is 537 mg/kg.
Chlordiazepoxide is a drug that is very frequently involved in drug intoxication, including overdose.[20] Chlordiazepoxide overdose is considered a medical emergency and, in general, requires the immediate attention of medical personnel. The antidote for an overdose of chlordiazepoxide (or any other benzodiazepine) is flumazenil. Flumazenil should be given with caution as it may precipitate severe withdrawal symptoms in benzodiazepine-dependent individuals.
Interactions[edit]
Some of the major interactions involving Chlordiazepoxide are listed below.[21]
ACE inhibitors, Adrenergic neurone blockers, Angiotensin II receptor antagonists, Beta blockers, Calcium channel blockers, Clonidine, Diazoxide, Diuretics, Hydralazine, Methyldopa, Minoxidil, Nitrates, Sodium Nitroprusside - enhanced hypotensive effect
Alcohol, barbiturates, opiates, antihistamines, antipsychotics - increased sedative effect in combination with benzodiazapines.
Cimetidine - metabolism of benzodiazepines inhibited by cimetidine (increased plasma concentration)
Disulfiram - metabolism of benzodiazepines inhibited by disulfiram (increased sedative effects)
Fluvoxamine - plasma concentration of some benzodiazepines increased by fluvoxamine
Levodopa - benzodiazepines possibly antagonise effects of levodopa
Moxonidine - sedative effects possibly increased when benzodiazepines given with moxonidine
Olanzapine - increased risk of hypotension, bradycardia and respiratory depression when parenteral benzodiazepines given with intramuscular olanzapine
Phenytoin - benzodiazepines possibly increase or decrease plasma concentration of phenytoin
Rifampicin - metabolism of benzodiazepines possibly accelerated by rifampicin (reduced plasma concentration)
Sodium oxybate - benzodiazepines enhance effects of sodium oxybate (avoid concomitant use)
Pharmacology[edit]
Chlordiazepoxide acts on benzodiazepine allosteric sites that are part of the GABAA receptor/ion-channel complex and this results in an increased binding of the inhibitory neurotransmitter GABA to the GABAA receptor thereby producing inhibitory effects on the central nervous system and body similar to the effects of other benzodiazepines.[22] Chlordiazepoxide is anticonvulsant.[23]
There is preferential storage of chlordiazepoxide in some organs including the heart of the neonate. Absorption by any administered route and the risk of accumulation is significantly increased in the neonate. The withdrawal of chlordiazepoxide during pregnancy and breast feeding is recommended, as chlordiazepoxide rapidly crosses the placenta and also is excreted in breast milk.[24] Chlordiazepoxide also decreases prolactin release in rats.[25] Benzodiazepines act via micromolar benzodiazepine binding sites as Ca2+ channel blockers and significantly inhibit depolarization-sensitive Calcium uptake in animal nerve terminal preparations.[26] Chlordiazepoxide inhibits acetylcholine release in mouse hippocampal synaptosomes in vivo. This has been found by measuring sodium-dependent high affinity choline uptake in vitro after pretreatment of the mice in vivo with chlordiazepoxide. This may play a role in chlordiazepoxide's anticonvulsant properties.[27]
Pharmacokinetics[edit]
Chlordiazepoxide is a long-acting benzodiazepine drug. The half-life of Chlordiazepoxide is 5 – 30 hours but has an active benzodiazepine metabolite (desmethyldiazepam), which has a half-life of 36 – 200 hours.[28] The half-life of chlordiazepoxide increases significantly in the elderly, which may result in prolonged action as well as accumulation of the drug during repeated administration. Delayed body clearance of the long half-life active metabolite also occurs in those over 60 years of age, which further prolongs the effects of the drugs with additional accumulation after repeated dosing.[29]
History[edit]
Chlordiazepoxide (initially called methaminodiazepoxide) was the first benzodiazepine to be synthesized in the mid-1950s. The synthesis was derived from work on a class of dyes, quinazolone-3-oxides.[citation needed] It was discovered by accident when in 1957 tests revealed that the compound had hypnotic, anxiolytic, and muscle relaxant effects. Three years later chlordiazepoxide was marketed as a therapeutic benzodiazepine medication under the brand name Librium. Following chlordiazepoxide, in 1963 diazepam hit the market under the brand name Valium - and was followed by many further benzodiazepine compounds over the subsequent years and decades.[30]
In 1959 it was used by over 2,000 physicians and more than 20,000 patients. It was described as "chemically and clinically different from any of the tranquilizers, psychic energizers or other psychotherapeutic drugs now available." During studies, chlordiazepoxide induced muscle relaxation and a quieting effect on laboratory animals like mice, rats, cats, and dogs. Fear and aggression were eliminated in much smaller doses than those necessary to produce hypnosis. Chlordiazepoxide is similar to phenobarbital in its anticonvulsant properties. However, it lacks the hypnotic effects of barbiturates. Animal tests were conducted in the Boston Zoo and the San Diego Zoo. Forty-two hospital patients admitted for acute and chronic alcoholism, and various psychoses and neuroses were treated with chlordiazepoxide. In a majority of the patients, anxiety, tension, and motor excitement were "effectively reduced." The most positive results were observed among alcoholic patients. It was reported that ulcers and dermatologic problems, both of which involving emotional factors, were reduced by chlordiazepoxide.[31]
Chlordiazepoxide enabled the treatment of emotional disturbances without a loss of mental acuity or alertness. It assisted persons burdened by compulsive behavior who, amongst other behaviors, felt compelled to count the slats on venetian blinds upon entering a room.[32] In 1963, approval for use was given to diazepam (Valium), a "simplified" version of chlordiazepoxide, primarily to counteract anxiety symptoms. Sleep-related problems were treated with nitrazepam (Mogadon), which was introduced in 1965, temazepam (Restoril), which was introduced in 1969, and flurazepam (Dalmane), which was introduced in 1973.[33]
Recreational use[edit]
In 1963, Carl F. Essig of the Addiction Research Center of the National Institute of Mental Health stated that meprobamate, glutethimide, ethinamate, ethchlorvynol, methyprylon and chlordiazepoxide as drugs whose usefulness “can hardly be questioned.” However, Essig labeled these “newer products” as “drugs of addiction,” like barbiturates, whose habit-forming qualities were more widely known. He mentioned a 90-day study of chlordiazepoxide, which concluded that the automobile accident rate among 68 users was 10 times higher than normal. Participants' daily dosage ranged from 5 to 100 milligrams.[34]
Chlordiazepoxide is a drug of potential misuse and is frequently detected in urine samples of drug users who have not been prescribed the drug.[35]
Legal status[edit]
Internationally, chlordiazepoxide is a Schedule IV controlled drug under the Convention on Psychotropic Substances.[36]
Toxicity[edit]
Animal[edit]
Laboratory tests assessing the toxicity of chlordiazepoxide, nitrazepam and diazepam on mice spermatozoa found that chlordiazepoxide produced toxicities in sperm including abnormalities involving both the shape and size of the sperm head. Nitrazepam, however, caused more profound abnormalities than chlordiazepoxide.[37]
Availability[edit]
Chlordiazepoxide is available in various dosage forms, alone or in combination with other drugs, worldwide.[38]
See also[edit]
- Alcohol withdrawal syndrome
- Effects of long-term benzodiazepine use
- Benzodiazepine withdrawal syndrome
- Benzodiazepine dependence
- Benzodiazepine
References[edit]
^ Liljequist R, Palva E, Linnoila M (1979). "Effects on learning and memory of 2-week treatments with chlordiazepoxide lactam, N-desmethyldiazepam, oxazepam and methyloxazepam, alone or in combination with alcohol". International Pharmacopsychiatry. 14 (4): 190–8. PMID 42628..mw-parser-output cite.citation{font-style:inherit}.mw-parser-output q{quotes:"""""""'""'"}.mw-parser-output code.cs1-code{color:inherit;background:inherit;border:inherit;padding:inherit}.mw-parser-output .cs1-lock-free a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-lock-subscription a{background:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration{color:#555}.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration span{border-bottom:1px dotted;cursor:help}.mw-parser-output .cs1-hidden-error{display:none;font-size:100%}.mw-parser-output .cs1-visible-error{font-size:100%}.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-format{font-size:95%}.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-left{padding-left:0.2em}.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-right{padding-right:0.2em}
^ Walker SR (2012). Trends and Changes in Drug Research and Development. Springer Science & Business Media. p. 109. ISBN 9789400926592.
^ Ban TA (2006). "The role of serendipity in drug discovery". Dialogues in Clinical Neuroscience. 8 (3): 335–44. PMC 3181823. PMID 17117615.
^ Marshall KP, Georgievskava Z, Georgievsky I (June 2009). "Social reactions to Valium and Prozac: a cultural lag perspective of drug diffusion and adoption". Research in Social & Administrative Pharmacy. 5 (2): 94–107. doi:10.1016/j.sapharm.2008.06.005. PMID 19524858.
^ "Chlordiazepoxide 10mg Capsules - Summary of Product Characteristics". UK Electronic Medicines Compendium. 19 December 2012. Retrieved 23 April 2017.
^ "Chlordiazepoxide". MedlinePlus Drug Information. February 15, 2017.
^ Liu GG, Christensen DB (2002). "The continuing challenge of inappropriate prescribing in the elderly: an update of the evidence". Journal of the American Pharmaceutical Association. 42 (6): 847–57. doi:10.1331/108658002762063682. PMID 12482007.
^ Authier N, Balayssac D, Sautereau M, Zangarelli A, Courty P, Somogyi AA, Vennat B, Llorca PM, Eschalier A (November 2009). "Benzodiazepine dependence: focus on withdrawal syndrome". Annales Pharmaceutiques Francaises. 67 (6): 408–13. doi:10.1016/j.pharma.2009.07.001. PMID 19900604.
^ Iqbal MM, Aneja A, Fremont WP (May 2003). "Effects of chlordiazepoxide (Librium) during pregnancy and lactation". Connecticut Medicine. 67 (5): 259–62. PMID 12802839.
^ Iqbal MM, Sobhan T, Ryals T (January 2002). "Effects of commonly used benzodiazepines on the fetus, the neonate, and the nursing infant". Psychiatric Services. 53 (1): 39–49. doi:10.1176/appi.ps.53.1.39. PMID 11773648.
^ Kripke DF (February 2016). "Mortality Risk of Hypnotics: Strengths and Limits of Evidence". Drug Safety. 39 (2): 93–107. doi:10.1007/s40264-015-0362-0. PMID 26563222.
^ drugs. "Chlordiazepoxide patient advice including side-effects". drugs.com. Retrieved April 7, 2008.
^ Nabeshima T, Tohyama K, Ichihara K, Kameyama T (November 1990). "Effects of benzodiazepines on passive avoidance response and latent learning in mice: relationship to benzodiazepine receptors and the cholinergic neuronal system". The Journal of Pharmacology and Experimental Therapeutics. 255 (2): 789–94. PMID 2173758.
^ McNamara RK, Skelton RW (March 1992). "Assessment of a cholinergic contribution to chlordiazepoxide-induced deficits of place learning in the Morris water maze". Pharmacology Biochemistry and Behavior. 41 (3): 529–38. doi:10.1016/0091-3057(92)90368-p. PMID 1316618.
^ Antkiewicz-Michaluk L, Grabowska M, Baran L, Michaluk J (1975). "Influence of benzodiazepines on turnover of serotonin in cerebral structures in normal and aggressive rats". Archivum Immunologiae Et Therapiae Experimentalis. 23 (6): 763–7. PMID 1241268.
^ Crawley JN, Marangos PJ, Stivers J, Goodwin FK (January 1982). "Chronic clonazepam administration induces benzodiazepine receptor subsensitivity". Neuropharmacology. 21 (1): 85–9. doi:10.1016/0028-3908(82)90216-7. PMID 6278355.
^ Committee on the Review of Medicines (March 1980). "Systematic review of the benzodiazepines. Guidelines for data sheets on diazepam, chlordiazepoxide, medazepam, clorazepate, lorazepam, oxazepam, temazepam, triazolam, nitrazepam, and flurazepam". British Medical Journal. 280 (6218): 910–2. doi:10.1136/bmj.280.6218.910. PMC 1601049. PMID 7388368.
^ MacKinnon GL, Parker WA (1982). "Benzodiazepine withdrawal syndrome: a literature review and evaluation". The American Journal of Drug and Alcohol Abuse. 9 (1): 19–33. doi:10.3109/00952998209002608. PMID 6133446.
^ Moretti M, Montali S (September 1982). "[Fetal defects caused by the passive consumption of drugs]". La Pediatria Medica E Chirurgica. 4 (5): 481–90. PMID 6985425.
^ Zevzikovas A, Kiliuviene G, Ivanauskas L, Dirse V (2002). "[Analysis of benzodiazepine derivative mixture by gas-liquid chromatography]". Medicina. 38 (3): 316–20. PMID 12474705.
^ British National Formulary. "Chlordiazepoxide interactions". BNF. Retrieved 7 Apr 2008.
^ Skerritt JH, Johnston GA (May 1983). "Enhancement of GABA binding by benzodiazepines and related anxiolytics". European Journal of Pharmacology. 89 (3–4): 193–8. doi:10.1016/0014-2999(83)90494-6. PMID 6135616.
^ Chweh AY, Swinyard EA, Wolf HH, Kupferberg HJ (February 1985). "Effect of GABA agonists on the neurotoxicity and anticonvulsant activity of benzodiazepines". Life Sciences. 36 (8): 737–44. doi:10.1016/0024-3205(85)90193-6. PMID 2983169.
^ Olive G, Dreux C (January 1977). "[Pharmacologic bases of use of benzodiazepines in peréinatal medicine]". Archives Francaises De Pediatrie. 34 (1): 74–89. PMID 851373.
^ Grandison L (1982). "Suppression of prolactin secretion by benzodiazepines in vivo". Neuroendocrinology. 34 (5): 369–73. doi:10.1159/000123330. PMID 6979001.
^ Taft WC, DeLorenzo RJ (May 1984). "Micromolar-affinity benzodiazepine receptors regulate voltage-sensitive calcium channels in nerve terminal preparations" (PDF). Proceedings of the National Academy of Sciences of the United States of America (PDF). 81 (10): 3118–22. doi:10.1073/pnas.81.10.3118. PMC 345232. PMID 6328498.
^ Miller JA, Richter JA (January 1985). "Effects of anticonvulsants in vivo on high affinity choline uptake in vitro in mouse hippocampal synaptosomes". British Journal of Pharmacology. 84 (1): 19–25. doi:10.1111/j.1476-5381.1985.tb17368.x. PMC 1987204. PMID 3978310.
^ Ashton CH. (April 2007). "Benzodiazepine equivalency table". Retrieved September 23, 2007.
^ Vozeh S (November 1981). "[Pharmacokinetic of benzodiazepines in old age]". Schweizerische Medizinische Wochenschrift. 111 (47): 1789–93. PMID 6118950.
^ Cooper JR, Bloom FE, Roth RH (January 15, 1996). The Complete Story of the Benzodiazepines (seventh ed.). USA: Oxford University Press. ISBN 0-19-510399-8. Archived from the original on 2008-03-18. Retrieved 7 Apr 2008.
^ New York Times (28 February 1960). "Help For Mental Ills (Reports on Tests of Synthetic Drug Say The Results are Positive)". The New York Times. USA. p. E9.
^ New York Times (28 August 1960). "Makers Worried On Tranquilizers". The New York Times. USA. p. F1.
^ Sternbach LH (June 1972). "The discovery of librium". Agents and Actions. 2 (4): 193–6. doi:10.1007/BF01965860. PMID 4557348.
^ New York Times (30 December 1963). "Warning Is Issued On Tranquilizers". The New York Times. USA. p. 23.
^ Garretty DJ, Wolff K, Hay AW, Raistrick D (January 1997). "Benzodiazepine misuse by drug addicts". Annals of Clinical Biochemistry. 34 ( Pt 1) (Pt 1): 68–73. doi:10.1177/000456329703400110. PMID 9022890.
^ Psychotropic Substances. New York: United Nations International Narcotics Control Board. 2016. p. 27. ISBN 978-92-1-048165-6.
^ Kar RN, Das RK (1983). "Induction of sperm head abnormalities in mice by three tranquilizers". Cytobios. 36 (141): 45–51. PMID 6132780.
^ Drugs.com Drugs.com: International availability of chlordiazepoxide Page accessed April 24, 2015
External links[edit]
- Rx-List.com - Chlordiazepoxide
- Inchem.org - Chlordiazepoxide
- U.S. National Library of Medicine: Drug Information Portal - Chlordiazepoxide
Categories:
- Amine oxides
- Benzodiazepines
- Chloroarenes
- GABAA receptor positive allosteric modulators
- Hoffmann-La Roche
(window.RLQ=window.RLQ||).push(function(){mw.config.set({"wgPageParseReport":{"limitreport":{"cputime":"0.988","walltime":"1.176","ppvisitednodes":{"value":7329,"limit":1000000},"ppgeneratednodes":{"value":0,"limit":1500000},"postexpandincludesize":{"value":232084,"limit":2097152},"templateargumentsize":{"value":9768,"limit":2097152},"expansiondepth":{"value":14,"limit":40},"expensivefunctioncount":{"value":4,"limit":500},"unstrip-depth":{"value":1,"limit":20},"unstrip-size":{"value":104021,"limit":5000000},"entityaccesscount":{"value":3,"limit":400},"timingprofile":["100.00% 928.334 1 -total"," 49.29% 457.544 1 Template:Drugbox"," 38.48% 357.249 1 Template:Infobox"," 36.45% 338.376 1 Template:Reflist"," 25.55% 237.184 26 Template:Cite_journal"," 9.29% 86.200 16 Template:Unbulleted_list"," 5.77% 53.591 1 Template:Infobox_drug/chemical_formula"," 4.98% 46.185 3 Template:Navbox"," 4.10% 38.097 1 Template:IPAc-en"," 3.81% 35.393 1 Template:Citation_needed"]},"scribunto":{"limitreport-timeusage":{"value":"0.426","limit":"10.000"},"limitreport-memusage":{"value":7500689,"limit":52428800}},"cachereport":{"origin":"mw1274","timestamp":"20181105230316","ttl":1900800,"transientcontent":false}}});mw.config.set({"wgBackendResponseTime":1279,"wgHostname":"mw1274"});});

 Clash Royale CLAN TAG
Clash Royale CLAN TAG